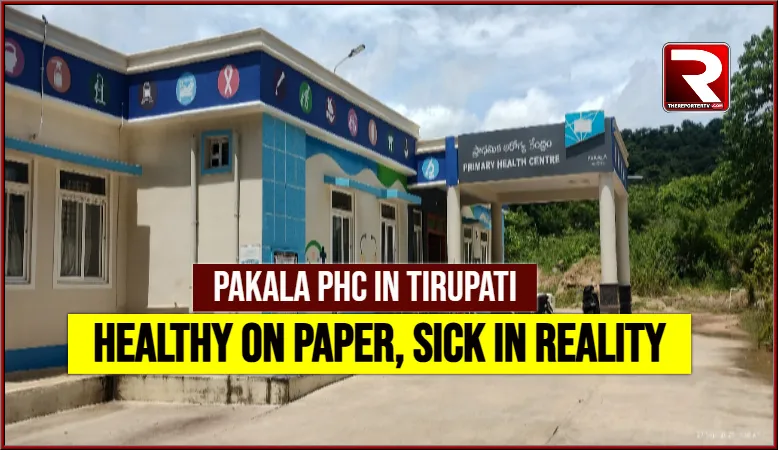
Pakala, Tirupati District — What initially appears to be a well-maintained, highly efficient Primary Health Centre (PHC) in Pakala Mandal headquarters quickly turns into a place of disappointment and disbelief for patients who walk in with hopes of proper treatment.
At first glance, the Pakala Government PHC presents an impressive image — almost resembling a corporate hospital. Clean premises, a staff display board listing a full team of medical personnel, and a seemingly organized setup give visitors confidence that they are in safe hands.
However, the illusion doesn’t last long.
Upon spending some time inside, the harsh reality begins to unfold. Patients and visitors start to question, “Why does this hospital look healthy but feel so sick inside?” A closer look reveals a shocking truth: the staffing list is more fantasy than fact.
Staff on Paper, Not on Duty
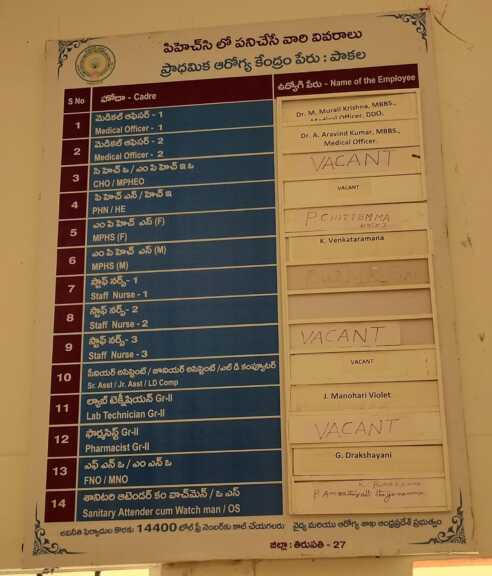
Official records displayed at the PHC list a comprehensive team:
-
1 Medical Officer
-
2 CHOs/MPHOs
-
1 PHN/HE
-
1 MPHS (F), 1 MPHS (M)
-
3 Staff Nurses
-
Senior and Junior Assistants
-
Lab Technician (Grade II)
-
Pharmacist (Grade II)
-
FNO/MNO
-
Sanitary Attendant-cum-Watchman/OAs
That’s a total of 14 types of healthcare and support staff.
But in reality?
Patients report seeing only one doctor and one nurse, who are forced to handle everything — from outpatient slips to patient care, from pharmacy duties to emergency responses. The nurse, in particular, is described as an “all-in-one” — managing roles well beyond her designated responsibilities.
When locals question the absence of the rest of the staff, the response is reportedly dismissive, almost sarcastic: “We are here, be happy with that.”
Treatment Quality: Half-Hearted and Incomplete
Due to the severe manpower shortage, patients say they receive only basic or incomplete treatments. Diagnostic services are minimal, follow-ups are rare, and the entire process leaves people feeling helpless.
One patient, visibly frustrated, said,
“This health centre needs treatment before it can treat anyone else. How can the government call this a functional PHC when it’s running on just two people?”
Public Disillusionment Growing
Patients leaving the centre express disappointment and concern over the situation, calling for immediate government attention.
“First give this health centre primary treatment, O Lord… it is the health centre itself that has become sick,” lamented a local woman.
This incident highlights the growing gap between government health schemes on paper and ground-level implementation, raising urgent questions about accountability, transparency, and the health of rural public healthcare infrastructure.
What Needs to Be Done
Locals are demanding:
-
A full audit of staff deployment and attendance
-
Regular inspections by district health officials
-
Immediate appointment of essential staff
-
Functional diagnostic and pharmacy services
Until then, what appears to be a model health centre will remain just that — a model, not a reality.